
Are you or a loved one facing breast cancer and seeking the best treatment options in Atlanta? At Radiotherapy Clinics of Georgia, we understand the challenges that come with a breast cancer diagnosis. Our advanced radiation therapy treatments offer hope and healing, in the Atlanta area.
There are several types of breast cancer treatment options available today thanks to years of ongoing breast cancer research. Here are some of the most common treatments.
A breast cancer treatment plan is created for each patient, specific to their type, stage and overall health condition. Your medical oncologist will work closely with the surgeon and radiation oncologists who will also be a part of many patients’ treatment program.
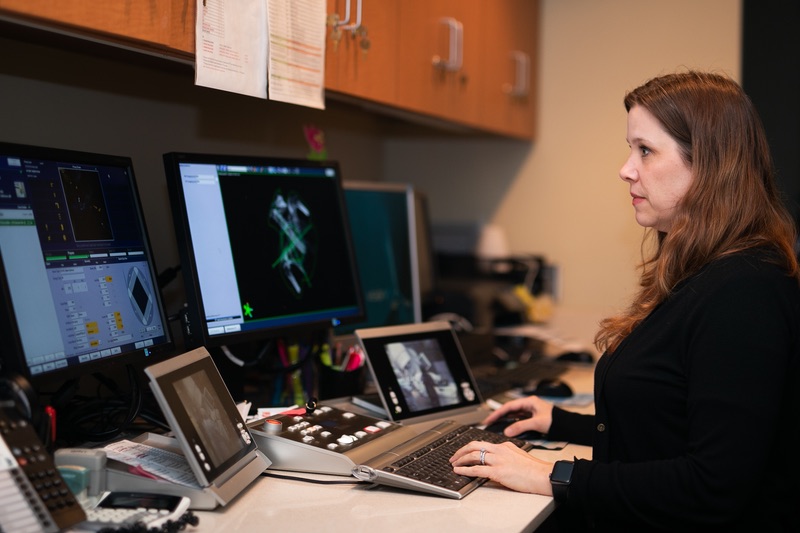
Breast cancer radiation therapy plays a vital role in the fight against breast cancer. At Radiotherapy Clinics of Georgia, we use the most advanced radiation therapy technologies to destroy cancer cells and prevent them from spreading.
Patients are often referred to receive radiation therapy at some point during their care, quite often right after surgery to be sure any left over breast cancer cells in the area are killed. You have a choice as to where you go. Talk to your medical oncologist about where you’d like to receive state of the art radiation therapy that’s also conveniently located near your home in the greater Atlanta region and surrounding areas including Athens and Augusta.
There are two types of radiation therapy used to treat breast cancer:
External radiation therapy
Internal radiation therapy
With external beam radiation, the radiation comes from an x-ray machine called a linear accelerator. To begin the treatment process, you will go through a planning session called a simulation. Those CT images are used to identify areas where treatment is needed and also areas that need to be protected, like the heart and lung. Your radiation oncologist will design and calculate a treatment plan tailored to your anatomy and the specifics of your breast cancer.
The radiation oncologist may use various planning techniques including IMRT (Intensity Modulated Radiation Therapy), 3D (three dimensional) or DIBH (Deep Inspiratory Breath Hold) to protect your organs. Once the plan is ready, you will undergo a practice session called a verification simulation to confirm your daily treatment setup.
Once the treatment begins your setup will be verified daily to ensure that the radiation is delivered to precisely the right place every time. IGRT (image-guided radiotherapy) may be utilized for the daily verification process. Treatments are delivered 5 days a week for 4 to 6 weeks. The treated area typically includes the whole breast and possibly the draining lymph nodes followed by treatment targeted to the lumpectomy cavity or mastectomy scar.
Related blog: What are the Types of Radiation for Treating Breast Cancer?
Hypofractionated radiation is external beam radiation that delivers the total dose of radiation in a shorter period of time. Clinical trials have proven hypofractionation to be just as safe and effective as conventional radiation therapy. Slightly larger doses are given during each treatment session so that the total number of days required to complete the course of treatment is shorter.
Hypofractionated radiation for breast cancer is delivered daily for 3-4 weeks. The standard treatment includes 42.5 Gray(Gy) over 16 daily fractions, the dosage may vary for each patient. The average daily treatment takes 30 minutes which includes time for check-in and out. Ask your radiation oncologist if you are a candidate for hypofractionated breast radiation therapy.
Before beginning external beam radiation therapy, your radiation oncologist will perform a physical examination. Afterward, a planning CT scan will be conducted, which is used for treatment mapping rather than diagnosis. The scan provides detailed images to help pinpoint the exact areas that require radiation targeting.
Your body may be marked with a small tattoo or a permanent marker to ensure accuracy during each session. These reference points help guide the radiation beams to the correct location. Additionally, a simulation session will take place before actual treatment begins. During this process, you will lie on the treatment table while the oncologist carefully aligns everything according to your personalized treatment plan, ensuring precision before the first dose is delivered.
Learn more about what to expect
Side effects from radiation treatment can vary, but there are some common side effects to watch for and talk to your oncologist and radiation technician who you will see often. They can often help you with treating the side effects and minimizing their effects. Since radiation is a targeted therapy side effects are limited to the treatment areas and not the entire body.
Common side effects of external radiation for breast cancer include:
Tenderness to the touch, especially in the area where the radiation beam is pointed
Red, dry, tender, or itchy skin similar to a sunburn. Your health care team may advise you to avoid exposing the treated skin to the sun since it could make the skin changes worse
Swelling, which may feel like breast “heaviness”
General fatigue, even after your treatments are complete

Accelerated partial breast irradiation (APBI) is a high-dose internal radiation therapy which may be an option for patients with early-stage breast cancer.
APBI involves the surgeon implanting a thin, hollow tube called a catheter into the breast. This surgery is typically the second one, scheduled after the lumpectomy and confirming that the margins around the lumpectomy are clear of cancer cells.
At the end of the catheter, a balloon or multiple smaller catheters are expanded to fill the lumpectomy cavity. Once the catheter has been placed, there is a treatment planning session called a CT simulation. The CT images collected during the planning process are used to identify where the treatment is needed and areas that will need to be protected, like your chest wall and skin. Your radiation oncologist will design and calculate a treatment plan tailored to your anatomy and the catheter placement.
Treatments are given twice a day for five days for a total of ten treatments. The catheter treatment device remains in place for the duration of the treatment course requiring daily dressing changes by your care team. During treatment, a radioactive seed is inserted into the catheter tube so that it can deliver radiation to the lumpectomy cavity. It’s only left in place for about 5-10 minutes each time the treatment is administered. Once complete the radiation oncologist will deflate the catheter and remove the device in the office.
When it comes to breast cancer treatment in Atlanta, Radiotherapy Clinics of Georgia stands out for several reasons:
We're proud to offer our advanced breast cancer radiation therapy at several convenient locations throughout the Atlanta area.
Most patients with breast cancer have surgery to remove the cancer. Types of surgery include the following:
Breast-sparing surgery: An operation to remove the cancer and some normal tissue around it, but not the breast itself. Part of the chest wall lining may also be removed if the cancer is near it. This type of surgery may also be called lumpectomy, partial mastectomy, segmental mastectomy, quadrantectomy, or breast-conserving surgery.
Mastectomy: Surgery to remove the whole breast that has cancer. Some of the lymph nodes under the arm may be removed and checked for cancer as well. In some cases, a skin-sparing mastectomy may be an option. For this approach, your surgeon removes as little skin as possible. Some women may also get a double mastectomy in which both breasts are removed.
Some patients may receive some treatment before surgery such as chemotherapy to help shrink the tumor before it’s removed.
After surgery for breast cancer, some women may choose breast reconstruction. It may be done at the same time as the cancer removal surgery or later.
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. The drugs that treat breast cancer are usually given through a vein (intravenous) or as a pill. If chemotherapy is part of your treatment plan, you will probably receive a combination of drugs. Your medical oncologist along with the cancer care team will determine the chemotherapy regimen and follow-up needed.
Some anticancer drugs are known to damage the ovaries. Women who have not gone through menopause yet may experience side effects including hot flashes, vaginal dryness, irregular periods (or periods that stop altogether), and infertility (inability to become pregnant). For women over the age of 35, this damage to the ovaries is likely to be permanent.
On the other hand, you may remain able to become pregnant during chemotherapy. Before treatment begins, have a conversation with your doctor about birth control because many drugs given during the first trimester are known to cause birth defects.

If hormone receptors have been found on the breast cancer cells, hormone therapy can be used to slow or stop the cancer from growing or returning in the future.
Related blog: How Does The Type Of Breast Cancer Impact Treatments And Outcomes?
For women who have not yet gone through menopause, hormone therapy options include:
Tamoxifen: This drug can prevent the original breast cancer from returning and also helps prevent the development of new cancers in the other breast. Hormone therapy with tamoxifen is often given to patients with early localized breast cancer that can be removed by surgery and those with metastatic breast cancer (cancer that has spread to other parts of the body). The drug is given as a pill that is to be taken every day for five years. Typically, the side effects of tamoxifen mirror some of the symptoms of menopause, with the most common being hot flashes and vaginal discharge. Others are irregular menstrual periods, thinning bones, headaches, fatigue, nausea, vomiting, vaginal dryness or itching, irritation of the skin around the vagina, and skin rash. Serious side effects are rare, but they include blood clots, strokes, uterine cancer, and cataracts. You may want to read the NCI fact sheet on Tamoxifen.
LH-RH agonist: This type of drug can prevent the ovaries from making estrogen. It may be given by injection under the skin in the stomach area. LHRH is given to some premenopausal women who have just been diagnosed with hormone receptor-positive breast cancer. Side effects include hot flashes, headaches, weight gain, thinning bones, and bone pain. Examples are leuprolide and goserelin.
Surgery to remove your ovaries: The ovaries are a woman’s main source of estrogen until she goes through menopause. When the ovaries are surgically removed, this source of estrogen is also removed. (A woman who has gone through menopause wouldn’t benefit from this kind of surgery because her ovaries produce much less estrogen.) This results in immediate menopause. The side effects are often more severe than those caused by natural menopause. Your health care team can suggest ways to cope with these side effects.
If you have gone through menopause, your options include:
Aromatase inhibitor: Hormone therapy with an aromatase inhibitor is given to some postmenopausal women who have hormone receptor-positive breast cancer. Aromatase inhibitors decrease the body's estrogen by blocking an enzyme called aromatase from turning androgen into estrogen. Common side effects include hot flashes, nausea, vomiting, and painful bones or joints. Serious side effects include thinning bones and an increase in cholesterol. Anastrozole, letrozole, and exemestane are types of aromatase inhibitors.
Tamoxifen: Hormone therapy is given for at least 5 years. Women who have gone through menopause can expect to receive tamoxifen for 2 to 5 years. If tamoxifen is given for less than 5 years, then an aromatase inhibitor often is given to complete the 5 years. Some women have hormone therapy for more than 5 years. See above for more information about tamoxifen and its possible side effects.
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells. Targeted therapies usually cause less harm to normal cells than chemotherapy or radiation therapy do. Monoclonal antibodies, tyrosine kinase inhibitors, cyclin-dependent kinase inhibitors, mammalian target of rapamycin (mTOR) inhibitors, and PARP inhibitors are types of targeted therapies used in the treatment of breast cancer.
Drugs used in targeted therapy have been developed to target specific cell changes. Therefore, the drugs given to patients are usually based on their specific hormone status and the type of their breast cancer.
In about 1 in 5 women with breast cancer, the cancer cells have too much of a growth-promoting protein known as HER2 on their surface. HER2-positive breast cancers tend to grow and spread more aggressively. Different types of drugs have been developed that target the HER2 protein.
Trastuzumab (FDA-approved biosimilar forms are available)
Pertuzumab (Perjeta)
Pertuzumab, trastuzumab, and hyaluronidase–zzxf (Phesgo)
Neratinib (Nerlynx)
Ado-trastuzumab emtansine or T-DM1 (Kadcyla)
Ribociclib (Kisqali)
Olaparib (Lynparza)
Abemaciclib (Verzenio)
Alpelisib (Piqray)
Palbociclib (Ibrance)
Lapatinib (Tykerb)
Tucatinib (Tukysa)
Sacituzumab govitecan-hziy (Trodelvy)
Entrectinib (Rozyltrek) and larotrectinib (Vitrakvi)
Olaparib (Lynparza)
Talazoparib (Talzenna)
Immunotherapy uses medicines to stimulate a person's own immune system to find and destroy cancer cells. It uses materials made either by the body or in a laboratory to improve, target, or restore immune system function. Immunotherapy can be used to treat some types of breast cancer.

Quickly and efficiently build the materials you need to support your inbound marketing strategy. Drag and drop building blocks including testimonials, forms, calls-to-action, and more.