The prostate is located behind the pubic bones in a man’s pelvis and is sandwiched between the bladder on top and the rectum underneath. The purpose of normal prostate cells is to produce seminal fluid, which when mixed with sperm from the testicles is called semen – the white-colored fluid visible upon ejaculation. A normal-sized prostate is about the size of a walnut. Like a shell around an egg, a capsule covers and contains the prostate except at the apex (bottom). The urethra, a tube that runs through the middle of the prostate and out of the penis, empties urine out of the bladder. Very small tubes, called ejaculatory ducts, run from each testicle into the prostate and empty into the urethra in the middle of the gland. Prostate cells also secrete various proteins into the blood stream, one of which is called Prostate Specific Antigen (PSA).
PSA stands for Prostate Specific Antigen. The word ‘Specific’ means that this enzyme is produced only by prostate cells – whether normal prostate cells or prostate cancer cells. No other cells in the body – lung, intestine, liver, etc. – make PSA. The purpose of PSA is to keep semen (the white substance ejaculated during sexual intercourse) liquefied. PSA is also leaked into the bloodstream by normal prostate cells and can be measured by a simple blood test.
A Prostate Specific Antigen (PSA) test is a man’s best defense against prostate cancer because it can lead to early detection of prostate cancer, a critical part of being successfully treated. Recommendations for initiating testing for elevations or changes in PSA vary based on age, medical history and ethnicity. Current recommendations to start PSA testing include:
All Men over the age of 50
African American men 45 years old, or older
Men with a family history of prostate cancer at age 40
A rising PSA may be a sign of prostate cancer; however, a rising PSA may also be caused by Benign Prostatic Hyperplasia (BPH), an enlarged prostate.
Benign Prostatic Hyperplasia (BPH) is an enlarged prostate. A normal-sized prostate is about the size of a walnut; however, as a man ages, his prostate may grow. Urinary symptoms, such as a weak or slow stream, are normally caused from compression (squeezing) of the urethra due to an enlarged prostate.
Prostate cancer rarely causes any urine symptoms, such as a weak, slow stream. The urinary symptoms are normally caused from compression (squeezing) of the urethra due to an enlarged prostate, called Benign Prostatic Hyperplasia (BPH). The first sign or symptom of prostate cancer (other than an elevated PSA or positive digital rectal exam) is usually bone pain from cancer cells that have spread to bone, and this is a sign of advanced stage disease.
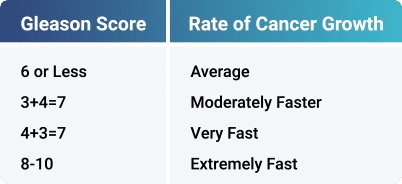
Gleason score predicts how fast prostate cancer is growing. It is the most important measurement in a pathology report. Gleason score consists of two numbers called grades, which range from 1-5. Grade 1 indicates slow growth prostate cancer, and grade 5 is rapidly growing cancer. The predominant grade seen in a needle core is the first number of the Gleason score. The second number is the next most common grade. These two grades are then added to get the Gleason score.
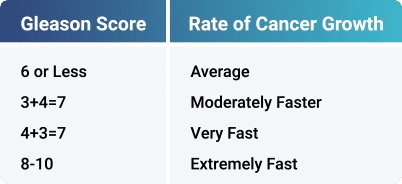
A 12-needle biopsy, which is the standard procedure for prostate biopsy, is sent to a pathology doctor who looks at the biopsy specimens under the microscope. Then, based upon his experience, he determines your Gleason score. Grade 1 indicates slow growth prostate cancer, and grade 5 is rapidly growing cancer. A Gleason score is based on the highest Gleason score number found in a biopsy, even if only in one needle. It is very common for men to have different Gleason scores in different areas of the prostate.
A rising Prostate Specific Antigen (PSA) and/or a positive digital rectal exam, conducted by your physician or other trained personnel, may indicate prostate cancer; however, a prostate biopsy is required to determine a diagnosis of prostate cancer.
Prostate cancer treatment methods are numerous, and most doctors will recommend the treatment method they perform. Prostate cancer treatment options include:
Radical Prostatectomy
Brachytherapy or seeds only, iodine or palladium
MRT/IGRT external beam radiation
ProstRcision – a combination of brachytherapy and external beam radiation
Hormones plus external beam radiation
Beam radiation first followed by iodine or palladium seeds
Iodine or palladium seeds followed by external beam radiation
HDR (High Dose Rate) seed radiation with external beam radiation
Cyberknife
Proton Beam Therapy
SBRT (Stereotactic Body Radiotherapy)
Cryosurgery
HIFU (High Intensity Focused Ultrasound)
Watchful Waiting or Active Surveillance (no treatment at all)
If you have been recently diagnosed with prostate cancer, it’s critical to personally research prostate cancer treatment options to make an informed decision that is best for you and your family. With few exceptions, your first treatment generally gives you the best chance for success.
For reasons unknown, one or more normal prostate cells transform into prostate cancer cells and begin to grow. The hallmark of any cancer is cancer cell growth – reproduction or making more cancer cells.
How a person develops prostate cancer is not known. It is assumed that something in the prostate causes one of the normal prostate cells to change into a cancer cell. Normal cells (prostate, liver, lung, etc.) have a balanced growth: when a new cell is made, an older one dies off, so the total cell number stays even. In contrast, cancer cells have uncontrolled growth. So, one cancer cell becomes two cancer cells, and those two cancer cells multiply to four cancer cells, then eight and so forth. And, since each prostate cancer cell usually makes a lot more PSA than a normal cell, they cause PSA in the bloodstream to elevate.
The purpose of normal prostate cells is to produce seminal fluid, which when mixed with sperm from the testicles is called semen – the white-colored fluid visible upon ejaculation.
A rising Prostate Specific Antigen (PSA) and/or a positive digital rectal exam, conducted by your physician or other trained personnel, may indicate prostate cancer; however, a prostate biopsy is required to determine a diagnosis of prostate cancer.
The most effective treatment for prostate cancer depends on the aggressiveness of the prostate cancer and the general health of the patient. If the growth of the prostate cancer is slow, watchful waiting, or no treatment at all, may be the best course of action until the cancer progresses. If the prostate cancer is aggressive, other treatment methods may be prescribed. If the prostate cancer has spread outside the prostate and metastasized, other treatments may be warranted.
Early detection of prostate cancer provides more treatment options and better outcomes. If you have been recently diagnosed with prostate cancer, it’s critical to personally research prostate cancer treatment options to make an informed decision that is best for you and your family. And, with few exceptions, your first treatment method gives you the best chance for success.
Proton therapy is a type of external beam radiation that targets the prostate cancer tumors with a stream of protons (small positively charged particles) instead of X-rays; it, therefore requires more specialized equipment. This type of radiation kills prostate cancer cells by altering the genetic material that controls how cells grow and divide with little damage to nearby tissues; although, healthy cells in the beam’s path are also damaged. At the present, despite the 10- to 20-fold increase in cost of the equipment, proton therapy has not been shown to be more effective than IMRT in tumor control.
If you have been recently diagnosed with prostate cancer, it’s critical to personally research prostate cancer treatment options to make an informed decision that is best for you and your family. And, with few exceptions, your first treatment method gives you the best chance for success.
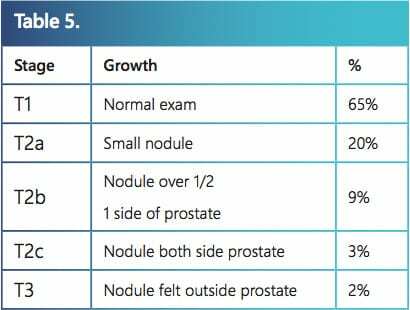
When evaluating a man’s particular case of prostate cancer, there are three major factors considered: 1) Gleason score 2) PSA and 3) stage. Stage is the third major factor for evaluation of a man’s prostate cancer. It is based strictly on finger examination of the prostate – the digital rectal examination or DRE. The table below lists the various stages and the percentage of men in these stages. Staging is the most inaccurate of the three major factors in evaluating prostate cancer because of microscopic capsule penetration.
The first step is the development of prostate cancer and growth inside the prostate gland. For reasons unknown, one or more normal prostate cells transform into prostate cancer cells and begin to grow. The hallmark of any cancer is cancer cell growth – reproduction or making more cancer cells. For a long period of time, prostate cancer grows only inside the prostate and is contained by the capsule that surrounds the prostate.
Eventually, the second step occurs – cancer cell leakage through the capsule outside the prostate, which is officially called microscopic capsule penetration. Depending upon the treatment method, prostate cancer can still be successfully treated in either Step 1 or Step 2. If left alone, Step 3 will eventually occur. The third step is the spread of prostate cancer (metastasis) beyond the area of the prostate such as lymph nodes, bones, lungs or any other place in the body. Step 3 is today considered incurable prostate cancer.
Your doctor or urologist may order a prostate biopsy if your PSA (prostate-specific antigen) test is elevated, or an abnormal lump is found on the prostate during a digital rectal exam. A prostate biopsy is normally about a 10-minute procedure and performed by a urologist. Twelve (12) needle samples are normally taken though the wall of the rectum (transrectal biopsy) but may be taken through the perineum (transperineal biopsy), the area between the anus and scrotum.
After the procedure, the 12 needle samples are sent to a pathologist for evaluation. The pathologist will determine how many of the needles contain cancer (if any) and the severity of the cancer and develop a Gleason score. The pathologist will write a pathology report and send it to your urologist.
Understanding the meaning of prostate cancer cure is one of the most important things learned while conducting research on prostate cancer. You are striving for a PSA of less than 0.2 ng/ml after several months of treatment and remain at that level for 10 years or more.
When found early, prostate cancer is treatable and long-term survivability rates are high; however, prostate cancer is unique for every individual. Treatments depend on the aggressiveness of the prostate cancer and whether the cancer is contained to the prostate.
From RCOG’s database, an individual cure rate can be provided by matching men who have a similar age, Gleason score, PSA, stage, and the number of needles positive for cancer.
There are over twelve treatment options for prostate cancer, some newer than others. Do you want to undergo a newer treatment or be treated with a prostate cancer treatment with documented survival rates?
ProstRcision® has high documented disease-free survival rates using the strictest definition (PSA less than 0.2 ng/ml, 10 years after treatment). This unique approach to eradicating prostate cancer preserves sexual function and maintains urinary control for the vast majority of men. The documented 10-year and 15-year high success rates, combined with no cutting of the prostate, and very few side effects are why over 16,000 men from all 50 states, and over 40 countries have chosen ProstRcision.
CyberKnife is a form of high-dose radiation treatment for prostate and other forms of cancer. CyberKnife’s unique robotic arm delivers Stereotactic Body Radiation Therapy (SBRT) to the prostate while compensating for movements of the prostate and, theoretically, protecting nearby tissue. The movement of the prostate is tracked through three to five tiny gold seeds known as fiducial markers that are inserted in the prostate through ultrasound-guided needles prior to radiation treatment. Treatment duration is normally four to five days. CyberKnife is a relatively new treatment method, and clinic trials are underway to determine CyberKnife’s long-term effectiveness and proper dosage levels.
If you have been recently diagnosed with prostate cancer, it’s critical to personally research prostate cancer treatment options to make an informed decision that is best for you and your family. And, with few exceptions, your first treatment method gives you the best chance for success.
A rising Prostate Specific Antigen (PSA) and/or a positive digital rectal exam, conducted by your physician or other trained personnel, may indicate prostate cancer; however, a prostate biopsy is required to determine a diagnosis of prostate cancer.
The aggressiveness of the prostate cancer, found during a prostate biopsy, and early or late detection determines the danger of prostate cancer. The early detection of slow growing prostate cancer provides better survivability rates than aggressive prostate cancer not detected early.
Life expectancy after a prostate cancer diagnosis depends of the aggressiveness of the cancer, or Gleason score, and early detection. If the cancer is slow growing, a man may die of other causes before he dies from prostate cancer.
ProstRcision® has high documented disease-free survival rates using the strictest definition (PSA less than 0.2 ng/ml, 10 years after treatment). This unique approach to eradicating prostate cancer preserves sexual function and maintains urinary control for the vast majority of men. The documented 10-year and 15-year high success rates, combined with no cutting of the prostate, and very few side effects are why over 16,000 men from all 50 states, and over 40 countries have chosen ProstRcision.
ProstRcision®, a combination of brachytherapy and external beam radiation, has high documented disease-free survival rates using the strictest definition (PSA less than 0.2 ng/ml, 10 years after treatment). This unique approach to eradicating prostate cancer preserves sexual function and maintains urinary control for the vast majority of men. The documented 10-year and 15-year high success rates, combined with no cutting of the prostate, and very few side effects are why over 16,000 men from all 50 states, and over 40 countries have chosen ProstRcision.
The aggressiveness of prostate cancer is different for each man and is determined by a prostate biopsy and the calculation of a Gleason score by a pathologist.
ProstRcision® is a combination of radioactive prostate seed implants and external beam radiation, where radiation doses for each have been fine-tuned over the last 30 years. ProstRcision has high documented disease-free survival rates using the strictest definition (PSA less than 0.2 ng/ml, 10 years after treatment). This unique approach to eradicating prostate cancer preserves sexual function and maintains urinary control for the vast majority of men. The documented 10-year and 15-year high success rates, combined with no cutting of the prostate, and very few side effects are why over 16,000 men from all 50 states, and over 40 countries have chosen ProstRcision.
Brachytherapy is a form of internal radiation used to treat prostate and other forms of cancer and involves placing devices containing radiation close to the cancer cells. Prostate brachytherapy may either be temporary or permanent. Temporary prostate brachytherapy treatment involves inserting radioactive wires into the prostate for a specific period of time, usually several minutes, before the wires are removed. During permanent prostate brachytherapy treatment, radioactive material is sealed inside seeds or capsules and implanted in and near the prostate cancer through ultrasound-guided needles and left in the prostate. The radiation given off by the wires or seeds damages the DNA of the cancer cells, preventing further cancer growth and killing the cancer cells.
If you have been recently diagnosed with prostate cancer, it’s critical to personally research prostate cancer treatment options to make an informed decision that is best for you and your family. And, with few exceptions, your first treatment method gives you the best chance for success.
ProstRcision® is a combination of radioactive prostate seed implants and external beam radiation, or Image-Guided Radiation Therapy (IGRT). IGRT treatments are similar to getting a pelvic x-ray each day. After a patient is placed on the accelerator table, the gold and I-125 seeds are targeted. The prostate is cross fired from multiple directions. After a man’s treatment is finished, which usually takes less than 10 minutes, he may go back to his normal daily activities. The patient returns the next day and the process is repeated. Beam irradiation treatments are given daily, Monday through Friday for a total of 30 to 35 treatments.
Decide which treatment methods gives you the best chance of maintaining a zero PSA for 15 years after treatment for your particular case of prostate cancer. There is no one cure rate for surgery because it varies with the skill of the urologist. Also, microscopic capsule penetration is probably a bigger problem for surgery than ProstRcision. You should also look at the other big issues: urinary incontinence and the loss of sexual function.
Make an informed prostate cancer treatment decision. Our 40-page, comprehensive guidebook provides answers to our most frequently asked questions from men diagnosed with prostate cancer, and compares various treatment methods, cure rates and side effects. Our team can also connect you with one of our oncologists at no cost.
Quickly and efficiently build the materials you need to support your inbound marketing strategy. Drag and drop building blocks including testimonials, forms, calls-to-action, and more.